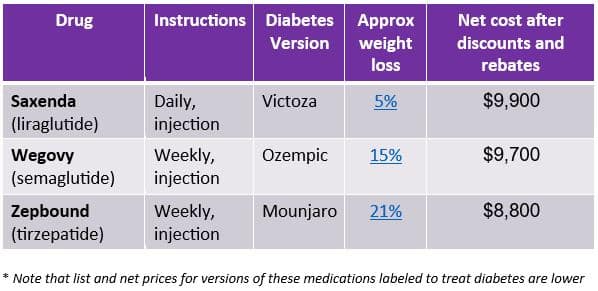
Ozempic, Wegovy, Mounjaro and Zepbound—GLP-1 drugs (also known as glucagon-like peptides) are the talk of social media, medical journals and among human resources professionals. These drugs are highly effective but terribly expensive, generally costing $8,000-$10,000 per patient annually, even after rebates and discounts. WTW surveys show that about four in 10 employers cover these drugs for obesity, and most cover them for diabetes. We estimate that the cost of GLP-1 drugs for obesity is currently about 10% of total pharmacy spending.
The path forward on GLP-1 coverage
Here are eight considerations for employers as they make choices about GLP-1 coverage.
1. GLP-1 drugs are highly effective and likely to be approved for new indications in addition to obesity and diabetes.
Weight losses of 15% or even 20% of body weight are common with the newer GLP-1 medications. Recent studies show that this class of drugs is effective in lowering risk of cardiovascular disease and improving sleep apnea and might be appropriate to treat fatty liver disease, Alzheimer’s disease, smoking cessation and substance use disorder. Although these drugs can improve health and prevent some future medical costs, their high prices and need for long-term use mean that they will not lower overall group health plan sponsor medical costs.
2. Weight regain is common after discontinuation of GLP-1 drugs.
The GLP-1 drugs are about as effective as bariatric surgery for weight loss, although weight regain is common after discontinuation. The largest semaglutide trial showed that patients regained two-thirds of lost weight in a year, although a study of electronic medical records showed regain of only a third of lost weight.
See also: 8 benefits areas HR is focusing on in 2024

Adherence is important to reaching goals. Pharmacy benefit managers report 50%-75% adherence at one year; members might stop the drugs due to side effects, drug shortages, plan design or utilization management programs. Some employers have announced lifetime maximums for GLP-1 drugs for obesity, which could impact long-term success. Lifetime and annual dollar limits are permitted currently on drugs that are not essential health benefits under the ACA, but the ability to apply these limits faces an uncertain future and should be monitored closely.
3. More GLP-1 drugs are coming, and some are more effective and convenient, which could bring more competition and potentially lower unit cost.
There are over 100 GLP-1 and related drugs currently under development. Many act on multiple different targets, and some have demonstrated up to 24% weight loss in clinical trials. One drug in trials would require only monthly injections, and many candidate drugs are oral. Approval of new medications will introduce competition and may lower unit cost. Lower unit cost could lead to more members taking these medications.
4. The GLP-1 medications have known side effects but are largely safe based on experience with diabetic patients and well-tolerated by most people.
Many people treated with these medications will have gastrointestinal side effects like nausea and constipation, and these often abate over time. Substantial weight loss from surgery, diet or these drugs leads to loss of lean body mass, and loss of fat tissue can accentuate facial wrinkles. This class of drugs has been used for almost two decades to treat diabetes, although it is possible new side effects will become evident with more users and newer drugs. There are reports of suicidality with use of these drugs, but a large observational study showed a statistically significantly lower rate of suicidal ideation compared to a matched group.
5. Many vendors promise to manage utilization of GLP-1 medications, but most programs are too new to have proven outcomes.

WTW is tracking over 40 weight loss vendor programs marketing to employers. Many have recently added the capability to prescribe drugs via limited prescriber networks, while others claim to “deprescribe” these drugs or use less expensive generic drugs prior to GLP-1s. Vendor solutions are typically app-driven with telephonic support and may leverage a wireless connected scale or wearable continuous glucose monitors. Program engagement may be a requirement for drug approval. Some incorporate bariatric evaluations and centers of excellence into their offerings as well. The cost of these programs varies widely and should be considered an additive cost to the drugs. Employers should consider integration of these types of third-party vendor solutions with their carrier and PBM medical management programs.
6. Benefit design and utilization management programs can lead to loss of rebates.
Employers that implement higher BMI requirements or “step” therapy to require programs or other drug therapy before GLP-1s for weight loss should consider rebate implications, as manufacturers may reduce or eliminate rebate payments on those drugs. These medications have high associated rebates, so employers should consider “net” cost rather than list price when evaluating economic impact of benefit design or management programs.
7. Medicare covers these drugs for diabetes and prevention of heart disease, but not for obesity.
Medicare is prohibited from covering weight loss drugs by legislation, but the Center for Medicare and Medicaid Services told Part D plans that they could provide coverage for GLP-1s for those with known heart disease. GLP-1 coverage for retiree plans should be carefully evaluated, especially with significant changes to Part D plans due to the Inflation Reduction Act.
8. GLP-1 drugs for obesity can impact health equity.
Widespread availability of anti-obesity drugs could increase health equity by improving medical outcomes for those with lower incomes who are more likely to have obesity. However, early evidence suggests that these drugs are used more frequently in predominately white, wealthy neighborhoods. Higher premium costs and higher out-of-pocket costs have greater impact on lower-wage employees. Employers can check with their counsel on compliance considerations around higher cost-sharing or lifetime maximums for these medications.
The GLP-1 drugs represent an enormous stride in improving metabolic health for those with obesity, but currently come at a very high price. Future prices are uncertain, and utilization is likely to increase as manufacturers produce more supply. Employers should continually reevaluate benefit design and programs for metabolic disease to keep their plans affordable and obtain maximum value for their members.
 *
*
From the authors: Thanks to Jeff Levin-Scherz, MD MBA, and Chantell Sell Reagan, PharmD, for their review and contributions.
The post Amid a changing landscape for GLP-1 drugs, 8 employer considerations appeared first on HR Executive.